Study identifies promising target for treating inflammatory bowel disease and colitis-induced colorectal cancers
Ting Fu
Inflammation in the gut can trigger a doom loop of sorts. The condition messes with the sensitive relationships between food, digestive acids, microbes and the immune system in ways that can promote further inflammation and, sometimes, the eventual growth of tumors.
Scientists at the University of Wisconsin–Madison have identified a promising new target for treatments that could help the millions of people worldwide who suffer from inflammatory bowel disease and related colorectal cancers.
An essential regulator of gut health
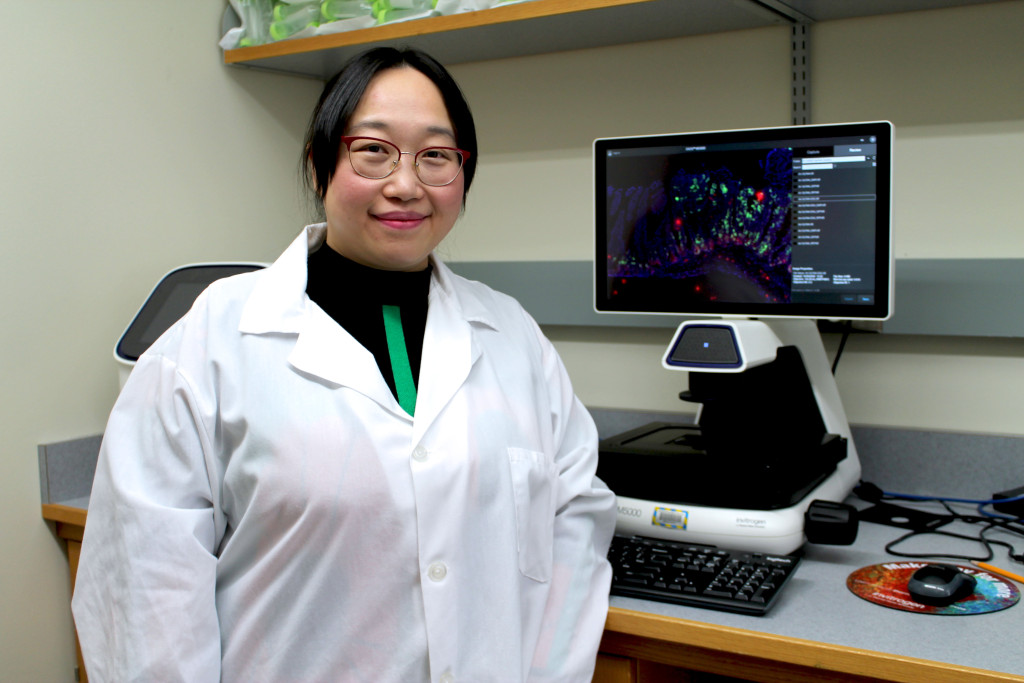
Under the guidance of Ting Fu, an assistant professor in the UW–Madison School of Pharmacy, researchers uncovered a previously unknown function of a protein that is central to gut health and implicated in the development of colitis, a severe and chronic form of IBD. A debilitating condition in and of itself, colitis is also linked to an increased risk for colorectal cancer. The team’s findings suggest that the protein is a promising target for future colitis treatments.
The protein is called the farnesoid X receptor, or FXR. It helps control the production of bile acids that digest fats. Working in tandem, FXR and bile acids play several critical roles in maintaining a healthy gut. Together, they help balance gut bacteria, promote a healthy intestinal lining, and influence immune cells called macrophages that patrol the digestive system and ward off pathogens that sneak in with the food we eat.
“This balance can be thrown off when FXR isn’t functioning properly,” says Xingchen Dong, a postdoctoral researcher in Fu’s lab and the study’s lead author.
Dong, Fu and their colleagues studied mice with chronic gastrointestinal inflammation that led to the growth of tumors in their colons. This mimicked the effects of colitis-associated colon cancer in humans. They found that FXR was not functioning properly in these mice, messing with the signals the protein sends to manage bile acids.
At the same time, they noted shifts in the chemistry of bile acids within the animals’ gastrointestinal tracts. These changes affected both “host” bile acids, produced by the mice themselves, and microbial bile acids, which are the product of gut microbes metabolizing host bile acids.
In a cascade of negative effects, the altered bile acids prompted changes in the behavior of gut macrophages, leading to a large increase in certain proteins called cytokines that promote inflammation. This observation provided compelling new evidence for how FXR dysfunction changes the behavior of gut macrophages, initiating the inflammation doom loop that can cause colitis and eventually lead to aggressive cancers.
From a scientific perspective, “it is exciting to see that gut macrophages have the capability to sense both host and microbial bile acids and exhibit diverse responses to various bile acids, which leads to changes in their state or activity,” says Fu.
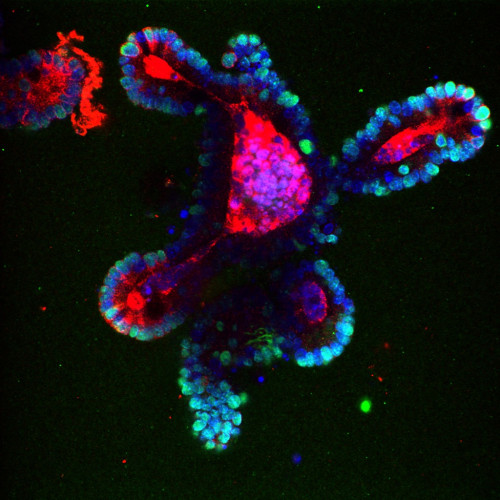
This image shows the effect of pro-inflammatory cytokines on the growth of a mouse intestinal organoid. Intestinal stem cells (red) are indicative of inflammation and Ki67 proteins (green) are associated with tumors. Photo courtesy of Ting Fu
A promising treatment for colitis and associated cancers
FXR dysfunction is implicated in a number of gastrointestinal diseases, and Fu’s team investigated whether existing drugs aimed at activating FXR — called FXR agonists — might prove effective treatments for colitis and associated colon cancers.
Mice treated with either of two FXR agonists — fexaramine D or FDA-approved obeticholic acid — saw marked improvement in FXR functioning, with a stream of other positive effects, including rebalanced bile acids, improved macrophage function and reduced intestinal inflammation.
Colorectal tumors in the treated mice were also “profoundly reduced” in both number and size, according to Fu. The median survival time of mice with colitis-associated cancer was twice as long in animals treated with the compounds compared to those that received no treatment. The findings were published Jan. 23 in the journal JCI Insight.
“This study shows that FXR plays a crucial role in regulating how macrophages behave in the gut,” says Fu. “This could be really important for developing new treatments for IBD and colitis-associated cancers.”
Fu intends to continue exploring compounds that promote FXR function as potential treatments for colitis and related cancers, though any treatment strategies for human patients based on this research will require further exploration and confirmation.
This work was funded by UW–Madison startup grants (AAI3795, AAI3894), UW Carbone Cancer Center startup support (AAI5122), UW Center for Human Genomics & Precision Medicine startup support (AAI5319), fall competition support from Wisconsin Alumni Research Foundation (AAL8735), as well as American Cancer Society institutional grant (AAH4826), and American Cancer Society – Coaches vs. Cancer – Bo Ryan-Jay Holliday Families FundResearch Scholar Grants (RSG-23-1150338-01) and the Margaret Q. Landenberger Research Foundation.