Relieving stress in insulin-producing cells protects against Type 1 diabetes
Removing a gene that manages stress within insulin-producing beta cells draws helpful attention from the immune system, protecting mice predisposed to Type 1 diabetes from developing the disease, a new University of Wisconsin–Madison study shows.
The study also found that changes discovered in the modified mouse beta cells are also present in human beta cells that manage to survive the widespread beta-cell death that characterizes Type 1 diabetes.
This gives the researchers hope that their findings, published today in the journal Cell Metabolism, may point to a potential new treatment that could be administered very early in the development of diabetes. Type 1 diabetes afflicts as many as 20 million people around the world, contributing to glaucoma, nerve damage, high blood pressure and stroke. In the United States, it shortens life expectancy by more than a decade.

Feyza Engin
“When we eat, our beta cells produce about 1 million molecules of insulin every minute to help maintain normal blood glucose levels,” says Feyza Engin, a UW–Madison professor of biomolecular chemistry and senior author of the new study. “That is a big and stressful job, especially for a part of these beta cells called the endoplasmic reticulum.”
The endoplasmic reticulum is like the cell’s warehouse staff. It folds the insulin protein molecules that a beta cell produces, packing them for shipping to other parts of the body. If something goes wrong with the protein folding process, the shipping process backs up or even stops, stressing the endoplasmic reticulum. A stress-response gene called Atf6 perks up when a cell is struggling with unfolded proteins. But if Atf6 can’t resolve the protein-folding problem, prolonged stress will eventually kill the cell.
Engin’s lab bred a line of diabetes-predisposed mice without the Atf6 gene in their beta cells. Instead of meeting their typical fate, those mice were protected from diabetes. Analysis of the genes expressed by their beta cells suggested the cells entered a state called senescence far ahead of schedule.
Senescence is a period of the cell’s life cycle in which it stops dividing and halts other normal cellular business. Senescing cells can cause problems for neighboring cells by releasing inflammatory messaging molecules that trigger an immune system response.
“We removed — knocked-out — the Atf6 gene in the beta cells in the pancreas of our mouse model of Type 1 diabetes, and they did not become diabetic,” Engin says. “Instead of dying off, these cells unexpectedly appear to go into an early senescence state that initiated a beneficial immune response and helped the cells survive an autoimmune attack.”
DNA damage, stress and aging can kick off senescence, which can draw an immune system response that cleans up the senescent cells. If the immune system fails to clear these cells, they accumulate and cause chronic inflammation and disease.
“The beta cells without Atf6 exhibit transient senescence and start releasing this group of proteins, including leukemia inhibitory factor, or LIF, that recruits protective immune cells called M2 macrophages,” Engin says.
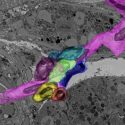
Macrophages are white blood cells that eat things — pathogens, foreign bodies, dead cells — that don’t belong in the body. In the pancreases of the Atf6-knockout mice, the M2 macrophages appeared to work around the altered beta cells, relieving inflammation and helping to reduce the accumulation of other, detrimental senescent cells. This led to healthier tissue and improved beta cell health and function, staving off Type 1 diabetes.
Even more exciting, Engin says, is how closely the new study’s results in mice appear to be reflected in human cells.
With a blood test, doctors can identify people who are at high-risk of developing Type 1 diabetes months in advance of the death of their beta cells.
“That may be a perfect timeframe for a treatment based on pharmacological inhibition of Atf6 or induction of LIF and other secreted proteins,” says Engin, whose work is funded by the National Institutes of Health. “If we can get there in time to protect these cells with transient senescence, the onset of diabetes might be prevented.”
While nearly all beta cells die off in diabetes, a few — though too few to be effective insulin suppliers — do survive. To see whether their mouse findings could be applicable in humans, Engin’s lab, with collaborators at Case Western Reserve University, Université Libre de Bruxelle and the University of Manitoba, studied beta cell samples taken from diabetes patients.
“In those surviving beta cells, we found reduced Atf6 activity and an early senescence gene expression pattern, suggesting this same process that kept our mice from becoming diabetic may have worked to protect these residual beta cells in humans,” Engin says.
The researchers hope to build on those findings by delving further into the role and potential benefits of senescence in Type 1 diabetes and other diseases.
This research was supported by grants from the National Institutes of Health (T32 GM007215, DK053307, DK060596, U01 DK127786, DK126444, DK133881-01, DK130919, DK128136), Juvenile Diabetes Research Foundation, Children’s Hospital Research Institute of Manitoba, Canadian Institutes of Health Research, Belgium’s Fund for Scientific Research, Dutch Diabetes Research Foundation and the Greater Milwaukee Foundation.
Tags: animal research, chemistry, research