With rat genome as guide, human breast cancer risk refined
Combing the genomes of the rat and the human, researchers at the University of Wisconsin–Madison have found swaths of genetic code that can be used to assess the risk of human breast cancer.
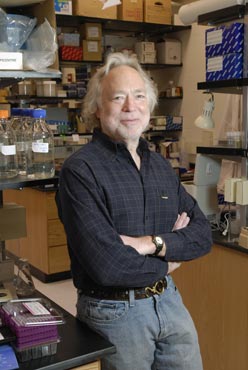
Michael N. Gould, oncologist with the McArdle Laboratory for Cancer Research at the University of Wisconsin–Madison, poses in his lab on March 19, 2007. Gould led a team of researchers that identified variations on regions of the human genome “that significantly associate with breast cancer research in women.” The team used Gould’s rat model for breast cancer to help identify the suspect areas of the human genetic code.
Photo: Aaron Mayes
The new work by a team of researchers at UW–Madison’s McArdle Laboratory for Cancer Research represents some of the early potential clinical payoffs of the massive efforts to gather and sequence the genomes of humans and other animals.
Writing in today’s (April 2) issue of the Proceedings of the National Academy of Sciences (PNAS), a team led by Wisconsin oncologist Michael N. Gould reports the discovery of genetic variations on regions of the human genome “that significantly associate with breast cancer risk in women.”
One of the newly identified regions of the human genome, known as a “resistance locus,” means that, on average, women who have it have a 15 percent decreased risk of breast cancer. Another region, which acts in a recessive manner, increases risk of disease by as much as 19 percent for the average woman.
The discovery is important because it could underpin new genetic screening methodologies for the most common type of cancer in American women. Instead of focusing on individual genes that may protect or predispose an individual to cancer, the new work demonstrates that identifiable patches of genetic code that do not always contain protein-making genes play a role in the onset of disease.
Unlike current genetic strategies for assessing breast cancer risk, which involve looking for mutations of two specific genes known as BRCA1 and BRCA2, the Wisconsin study identifies risk associated with areas of the genome that harbor so-called modifier genes, genes that do not make proteins, as many genes do, but instead act to influence other genes elsewhere on the genome and that help initiate the cascade of events that leads to breast cancer.
“Scientifically, this is unique, and we can use this new knowledge to study risk in the average woman,” says Gould. He adds that while mutations of the BRCA genes are good predictors of cancer risk in an individual, they are uncommon, occurring in less than 1 percent of women and are thus too rare to be used effectively for breast cancer screening. As many as 200,000 new cases of breast cancer are reported each year in the United States and upward of 50,000 people die annually as a result of the disease.
“This could be used to screen the general population,” says Gould of the work that utilized a rat model for breast cancer to find regions of the genome that seemed to influence the onset or prevent the disease. Knowing the regions of the rat genome important for breast cancer, Gould and his colleagues were able to identify similar regions on the human genome using data obtained from samples provided by nearly 12,000 women from Wisconsin and the United Kingdom.
The genetic variations found by Gould and his team occur on a portion of the genome that has no obvious direct function, such as making proteins. The implication is that the swath of genetic code identified by the Wisconsin group contains modifier components of the genome, which act at a distance to influence what other genes do.
Scientists believe that breast cancer and many other diseases result from a complex series of genetic events. They suspect that modifier loci play a big role in many types of diseases, but finding such genes has proved exceptionally difficult, Gould says. Thus, the new work adds an important new piece to the molecular puzzle of breast cancer and, according to Gould, is a strategy that is also now being employed to unravel the secrets of other diseases such as diabetes.
The rat model for breast cancer, developed by Gould’s lab during the past decade, provides a unique window to the molecular levers that influence disease. The rat is a good model for breast cancer because the disease manifests itself in the animal in much the same way it occurs in humans.
Using the model, Gould’s team was able to home in on eight areas of the rat genome that dispose or protect the animal from breast cancer. Then, scouring the human genome, it was possible to identify similar regions of genetic code that have been preserved throughout the course of evolutionary history.
“We scanned the whole genome of the animal (rat) model for breast cancer,” Gould explains. “We mapped several regions in the rat genome that were associated with susceptibility to mammary cancer.”
Using data from cancer patients, Gould’s team was then able to identify parts of the human genome that had similar variations that either increase or decrease the risk of disease.
An ability to screen women and assess breast cancer risk promises to help with prevention and early detection of the disease. Gould also believes that the knowledge may help spur new strategies for prevention and treatment.
“At the end of the day, not only have we found these markers in humans, but we have the animal model to test prevention and treatment strategies,” he says.
The work in Gould’s lab was spearheaded by David J. Samuelson, Stephanie E. Hesselson and Amy Trentham-Dietz. Bruce A. Ponder of the University of Cambridge is also a senior author of the new PNAS report. The work was funded primarily by the National Institutes of Health.
Tags: biosciences, breast cancer, cancer, genetics, research




