Some lymphomas become resistant to treatment. Gene discovery may offer path to overcome it.
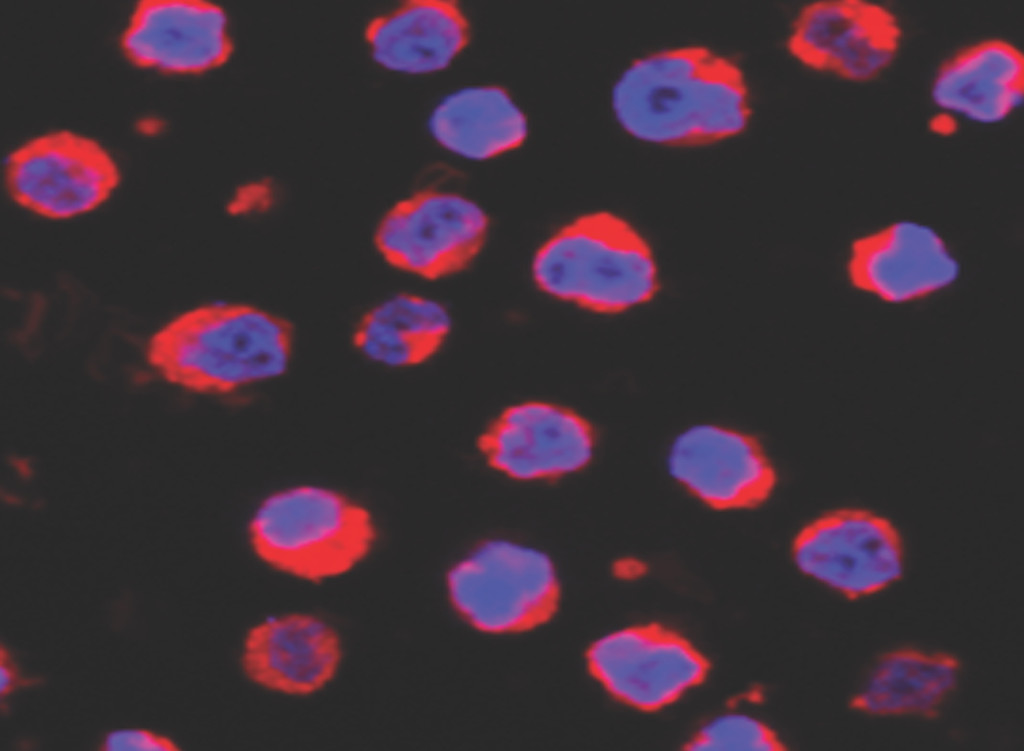
A confocal microscope image of lymphoma cells. It shows mitochondrial localization (red) around cell nuclei (blue). Image by: Lixin Rui
Patients with some types of lymphoma that become resistant to standard treatments may benefit from a therapy that University of Wisconsin–Madison researchers are evaluating after they discovered a key process that fuels the blood cancers’ resistance to current drugs. Here are the details:
An effective treatment, until it isn’t: The UW–Madison team sought to understand why some patients with certain non-Hodgkin’s lymphomas that originate in white blood cells called B cells develop resistance to drugs that have become a standard of care for the disease.
- Patients with B-cell malignancies, including mantle cell lymphoma and diffuse large B-cell lymphoma, often see their cancer initially respond well to treatments that include drugs called Bruton tyrosine kinase inhibitors, or BTK inhibitors.
- BTK inhibitors, including the commonly used drug ibrutinib, block B cells’ signaling pathway. This is helpful for treating B-cell lymphomas because the cancers arise when this signaling pathway malfunctions, leading to out-of-control production of B cells. BTK inhibitors short-circuit that overproduction.
- “However, most patients who respond to these drugs relapse after maybe one or two years of treatment. That’s a big issue,” says Lixin Rui, a professor of hematology, medical oncology and palliative care in the University of Wisconsin School of Medicine and Public Health, who led the research.
Identifying a new mechanism of resistance: Researchers have been trying to understand why and how BTK inhibitors often stop being effective, and Rui and his colleagues investigated resistance against ibrutinib specifically.
- Ibrutinib became the first BTK inhibitor approved to treat B-cell lymphomas in 2013 and remains one of the most widely prescribed drugs in the class for use against the cancers.
- The UW–Madison team performed genetic and pharmacological analyses that implicated a single gene in the development of ibrutinib resistance. The gene is responsible for producing a protein known as early growth response 1, or EGR1.
- The EGR1 protein serves a number of biological functions, including the regulation of cell proliferation. Rui and his colleagues found that the ibrutinib-resistant malignant B cells they examined displayed more active EGR1 genes than cells that weren’t resistant to the drug.
- This activity became even more pronounced following treatment with ibrutinib, as EGR1 promoted a cascade of changes to the cells’ metabolisms, increasing their energy.
- “This is a novel mechanism that we identified,” says Rui. “EGR1 can promote more energy production in resistant lymphoma cells and, therefore, it promotes drug resistance.” The discovery was recently detailed in the journal Blood.
Overcoming relapse: Figuring out how cancerous B cells gain resistance to BTK inhibitors like ibrutinib was only part of the goal of the UW–Madison team, which is ultimately seeking new effective treatments for lymphoma patients who have relapsed thanks to drug resistance.
- In the same study, Rui and his colleagues tested a new treatment regimen aimed at counteracting the overactivity of EGR1.
- The team landed on an experimental treatment involving two drugs that lower cells’ metabolisms: metformin, which is used to treat Type 2 diabetes, and a newer drug called IM156.
- In combination, these two drugs effectively slowed the growth of ibrutinib-resistant lymphoma cells in mouse models with drug-resistant B-cell lymphomas.
Eventually, Rui is hopeful the experimental treatment can make its way to clinical trials with human patients. “I always want findings from my lab translated to the clinic,” Rui says. “If patients can benefit from this research, that would be very rewarding.”
This research was supported by the National Institutes of Health, National Cancer Institute (R01 CA266354), UW–Madison Forward Lymphoma Fund, ASH Bridge Grant, UW Center for Human Genomics and Precision Medicine SeedGrant, Midwest Athletes Against Childhood Cancer, Inc. Fund, UW Carbone Cancer Center pilot grant NIH, NCI (P30 CA014520) and the Intramural Research Program of the NIH, NCI.