Drug protects fertility and may prolong life in chemo-treated mice
A University of Wisconsin–Madison physician and her research team have shown that a heart medication can prevent ovarian damage and improve survival in adolescent mice after chemotherapy. The treatment also increased the number of their healthy offspring.
If the repurposed heart medication — dexrazoxane, or dexra for short — has the same effects in people, it could save young lives while also overcoming limitations to fertility treatments currently used during cancer treatment, reports Sana Salih, an assistant professor of obstetrics and gynecology at the University of Wisconsin School of Medicine and Public Health.
Sana Salih works in her research lab at the UWClinical Science Center. Photo: UW Health
The study was published today in the scientific journal PLOS ONE.
Salih and her colleagues set out to find a better way to protect the fertility of young female cancer patients. “Fertility preservation following chemotherapy for children and women diagnosed with cancer is a formidable challenge,” she says. “For pre-pubescent girls, the only option to prevent chemo-induced ovarian failure is to preserve ovarian tissue by freezing.” Unfortunately, she adds, that is an experimental procedure that requires surgery to harvest and again to re-implant the tissue after cancer treatment. Such transplantation carries a small risk of cancer recurrence and provides only a short-term solution. “The transplanted ovarian tissue can only function for three to seven years,” Salih says.
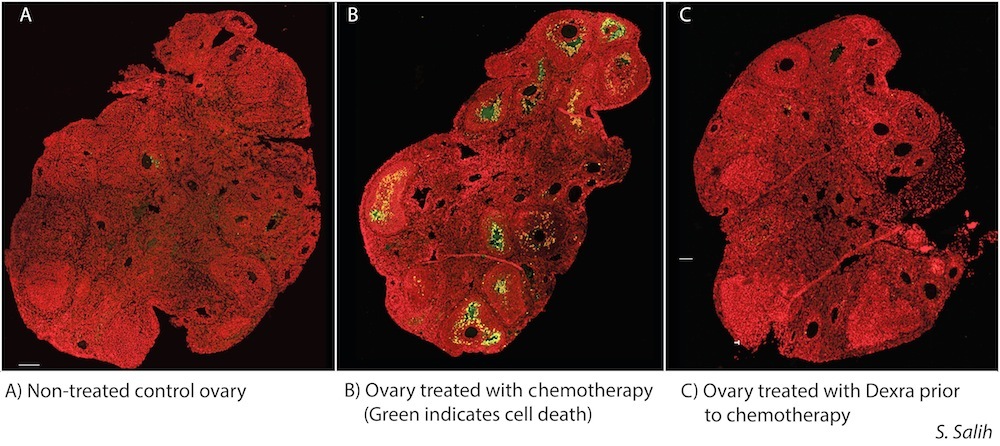
Salih was pleased to discover that administering dexra to mice before their ovaries were exposed to the chemotherapy agent doxorubicin (DXR) resulted in diminished ovarian damage and preserved ovarian function and fertility.
“What really surprised us is that a very small dose of dexra was enough to give full ovarian protection,” Salih says. Mice treated with dexra also gave birth to healthier litters, with more pups and higher birth weights than those that received DXR alone, she discovered.
Then came even more surprises: The dexra-protected mice given chemo lived much longer than mice given chemo only. Furthermore, mice given only dexra lived longer than even control mice receiving no interventions.
“The FDA currently limits the use of dexra to adults to protect their hearts from the toxic side effects of chemotherapy,” Salih said. “But these patients are receiving very high doses of dexra that may actually be contributing to increased toxicity, leading to decreased survival in some patients.”
The researchers achieved high mouse survival rates, ovarian protection and birthing successes using a dose of dexra 10 times lower than what is used for adult human cardiac protection. Post-mortem studies on the mice showed protection of ovarian, heart, and other cells and tissues.
“This is exciting,” Salih said. “We are now submitting a grant to look at low-dose dexra protection in nonhuman primates as a stepping stone to clinical translation in pediatric cancer patients.”
Salih, who directs the Oncofertility Program in the School of Medicine and Public Health, has begun studies needed to show that safe doses of dexra can protect developing primate ovaries. Nonhuman primate ovarian development, cycle time and gestation are very similar to that of humans.
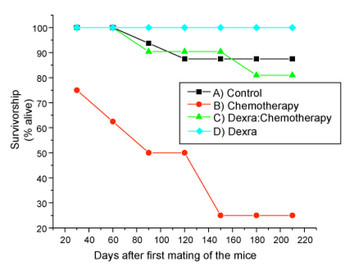
The red line indicates that most of the chemotherapy-only treated mice had extremely low survival rates; however, 90 percent of those treated with a low dose of dexra (green line) before chemotherapy lived much longer.
Source: Sana Salih
“My goal is to present data so that physicians can come up with dosage recommendations and safety profiles for early clinical trials in humans,” Salih says. “Up to 6 percent of young girls with childhood cancers and 50 percent of women with breast cancer who endure chemotherapy face ovarian failure. We need to give more cancer survivors real hope that they can conceive a healthy child.”
“The future of this research is to find more ways to protect not only the ovaries, but other tissues and organs as part of cancer treatment, to increase overall health and survival,” she says.
The paper’s authors include Elon Roti Roti (cq), an assistant scientist in Salih’s lab; post doctoral trainee Jenna Kropp and David Abbott, professor of obstetrics and gynecology, both at the Wisconsin National Primate Research Center. A Wisconsin Alumni Research Foundation grant, NIH Training Award, and University of Wisconsin Carbone Cancer Center Support Grant funded the research.
Tags: animal research, cancer, drugs, research