A UW biochemistry researcher is studying effective treatments for the next pandemic. Federal funding changes are slowing the work.
Biochemistry professor Robert Kirchdoerfer: “Innovative discovery is not something that you can just turn on and off.” Photo: Althea Dotzour
Research at the University of Wisconsin–Madison drives innovation, saves lives, creates jobs, supports small businesses, and fuels the industries that keep America competitive and secure. It makes the U.S.—and Wisconsin—stronger. Federal funding for research is a high-return investment that’s worth fighting for. Learn more about the impact of UW–Madison’s federally funded research and how you can help.
Behind every new drug and effective vaccine for infectious diseases lie years of research by scientists dedicated to building a foundational understanding of pathogens that could pose a threat to the public. Robert Kirchdoerfer, a biochemistry professor at the University of Wisconsin–Madison, has been studying the structure of coronaviruses like COVID-19 for years, while training the next generation of researchers who will work to prevent future pandemics.
With funding support from the National Institutes of Health, his lab analyzes the characteristics of coronaviruses to both understand how they work and inform the development of drugs that can protect against them.
We recently spoke with Kirchdoerfer to learn more about his work, how it’s being affected by federal funding changes, and the importance of student training opportunities.
Why do we need to continue researching coronaviruses, even if the COVID-19 pandemic has subsided?
While it may seem like the COVID-19 pandemic is over, researching this family of viruses is still vital. As we saw with the rapid appearance of SARS-CoV-2 variants, coronaviruses quickly mutate and adapt. They are incredibly adept at mixing and matching parts of their genomes through a process called recombination, creating new combinations of viral genes that can alter how the virus replicates or evades the host immune response. Since they can infect so many species — from humans to pigs to chickens — coronaviruses can replicate, mutate and become more infectious in many hosts.
How is your lab studying these coronaviruses?
We’re looking at this process called RNA (ribonucleic acid) proofreading. RNA is the genetic material coronaviruses copy to create more viruses. We normally think of RNA viruses as being super error-prone when they replicate their genomes. But coronaviruses are unique in that they actually have a proofreading enzyme to make fewer errors during genome replication. Proofreading also makes coronaviruses naturally resistant to many types of drugs normally used as broad-spectrum RNA virus antivirals. So, we’re looking at how that proofreading activity really works, as a prelude to figuring out how we can make better antiviral drugs to treat the next coronavirus pandemic.
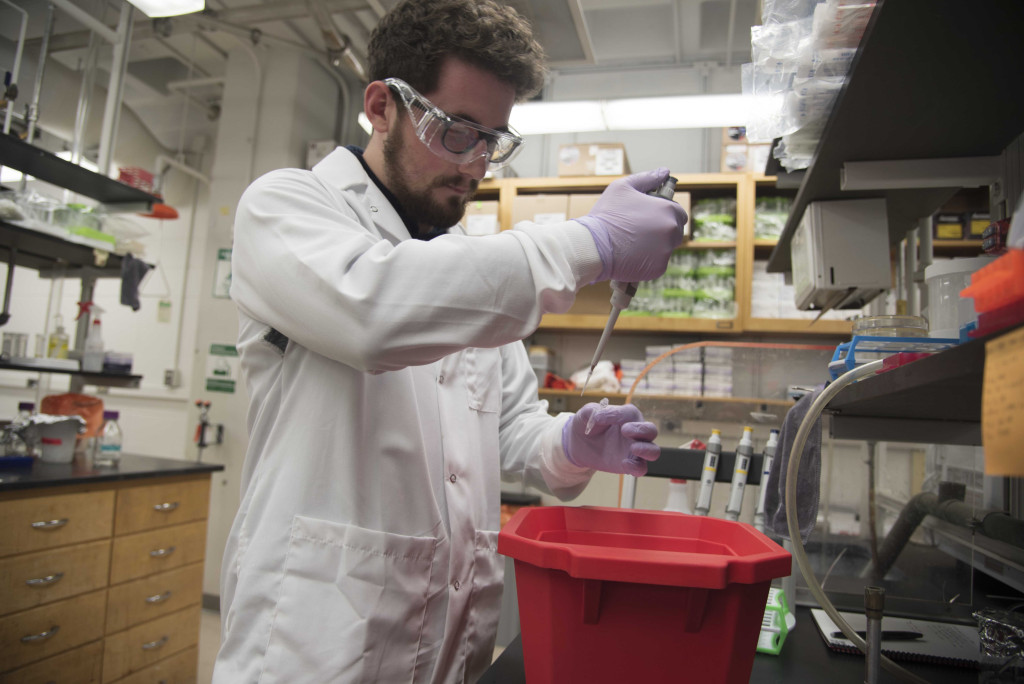
“The world’s ability to respond to tomorrow’s new virus is dependent on developing the highly skilled scientists that we are training today,” Kirchdoerfer says. Above, graduate researcher Thomas Anderson works with coronavirus enzymes in the Kirchdoerfer Lab. Photo: Andrew Leicht
What have you learned about the structure of coronaviruses?
We use a special imaging technology called cryo-electron microcopy to look at the structures of these viruses. Our work has shown that while coronaviruses from different host species may assemble their machinery in slightly different ways, the sites that are targeted by existing antiviral drugs are shared among these viruses. That means these antiviral drugs will likely be effective in treating coronavirus disease beyond just COVID-19. We’re currently examining how coronaviruses are naturally, broadly resistant to a class of antiviral drugs called nucleoside analogs.
Why was it possible to develop a vaccine for COVID-19 so quickly?
It doesn’t take eight months to make a vaccine or new drug — it takes five to 10 years or longer. We couldn’t have responded to COVID-19 as quickly as we did without years of foundational work. When science comes to the rescue during a public health emergency, that’s not because somebody went into a lab the next day and produced a cure. That’s because people worked on that science and treatment for 20 or 40 years. You need that long-term investment, training and development to be successful. Innovative discovery is not something that you can just turn on and off.
How has your research team been affected by changes in federal funding?
Luckily, I haven’t had to terminate any positions yet, but we have had to shut down some projects. Academic partners on campus or at other institutions used to contact us to test drug candidates. We would do biochemical assays, put it into our imaging analysis pipeline, figure out how those drugs work, and whether they really do work. But now we’ve had to shut down some of those projects because we don’t have the funding for the microscope time. We’ve really had to pare down the more collaborative studies in our lab.
How do funding changes affect student training in your lab?
My current students should graduate on their regular timelines, but there is going to be a reduction in the research program over the next five years. We’re not taking new students. And these students are at a unique time in their lives where if they can’t go to graduate school this year, there’s a good chance that they won’t go ever. That diverts people from this career path. Reduced participation in graduate programs means fewer PhDs and fewer quality, qualified people entering the biomedical workforce.
Why is student training so important?
University labs provide a training environment to teach up-and-coming scientists critical thinking, project management and other skills to perform scientific experiments. The world’s ability to respond to tomorrow’s new virus is dependent on developing the highly skilled scientists that we are training today.
Tags: federal relations, research




