UW–Madison researchers find hidden genetic clues upping cardiovascular disease risk
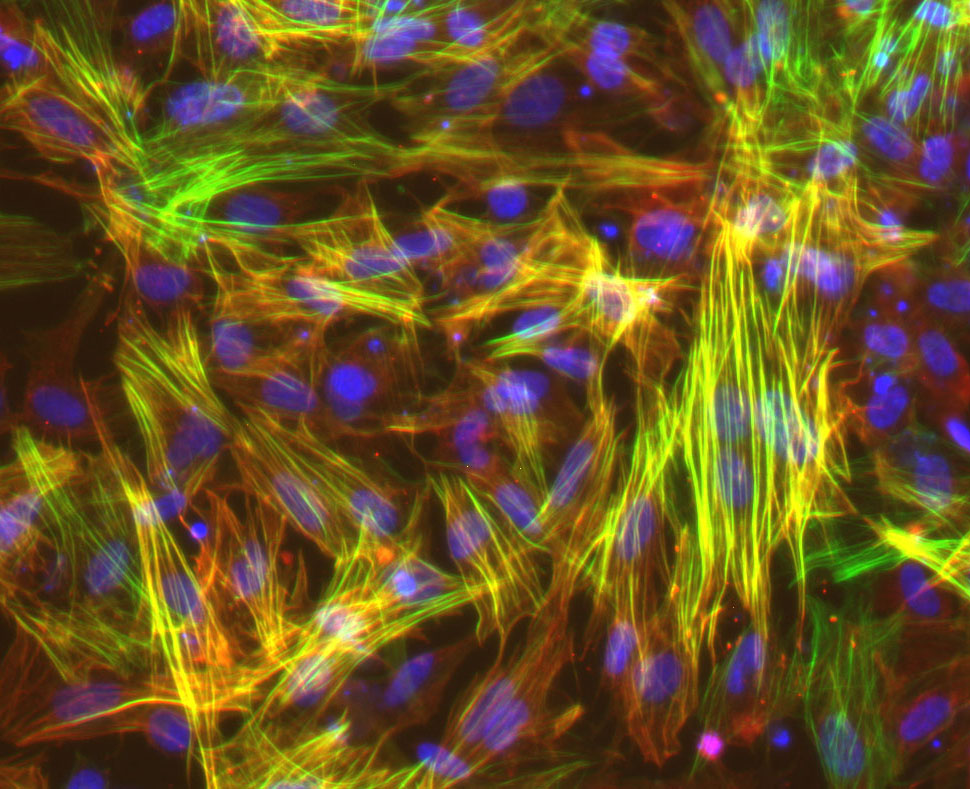
UW–Madison researchers studied smooth muscle cells like these, derived from induced pluripotent stem cells, to show that long-mysterious variations in an area of our genome harden blood vessels, puting some people at higher risk for cardiovascular disease. Image courtesy Lo Sardo Lab/UW–Madison
Researchers at the University of Wisconsin–Madison have uncovered new evidence in a decades-old genetic mystery, discovering how a group of genetic variations in a long-mysterious region of the human genome can put people at higher risk of cardiovascular disease.
Thanks to past studies of the whole human genome that drew associations between particular variations and disease, scientists have known for nearly 20 years that alterations in a section of human chromosome 9 called the 9p21.3 locus contribute to increased risk of developing coronary artery disease, CAD. The specific variations make atherosclerosis, a dangerous thickening and stiffening of the coronary arteries with plaque, more likely.
However, it was not well understood how the variations in this region lead to an increased risk for CAD. To solve that mystery, UW–Madison scientists coaxed induced pluripotent stem cells, which are living donor cells reprogrammed into a blank-slate state, into developing into the smooth muscle cells found in the walls of blood vessels.

Valentina Lo Sardo
In the lab of UW–Madison stem cell scientist Valentina Lo Sardo, genetics graduate student Elsa Salido found that smooth muscle cells carrying the risky version of 9p21.3 behaved differently than typical cells in healthy blood vessels, instead developing some of the features of cells seen in cartilage and bone.
“What we found is that the cells change their transcriptional makeup, and they are in between smooth muscle and these osteochondrogenic [or bone-like] cells. We discovered that these cells are more prone to calcification,” says Lo Sardo, lead researcher on the project and a professor of Cellular and Regenerative Biology in the UW School of Medicine and Public Health and member of UW–Madison’s Stem Cell and Regenerative Medicine Center. “This is very important, because CAD is basically atherosclerosis [a hardening of the arteries] and calcification of the arteries is one of the hallmarks of this type of pathology.”
Understanding how the change in the genome increases risk for CAD is a step toward potentially preventing its damaging effects and perhaps one day developing therapeutic strategies to block the risky changes in arteries. The researchers published their findings recently in the journal Arteriosclerosis, Thrombosis, and Vascular Biology.

Elsa Salido
By using genome editing to remove the disease-associated version of 9p21.3, the researchers were able to see that the cells revert to a “healthy” status, showing that disarming the risk effect of this genomic region may be valuable to reenabling smooth muscle cells to exert their function.
Lo Sardo notes that CAD is a complex disease influenced by multiple factors, including environmental factors, lifestyle choices and genetics. But, in the case of 9p21.3, the researchers discovered that variations in this genomic region can promote calcification without the influence of any outside factors. They also discovered that as the cells calcify more, they lose their ability to do healing remodeling, important to maintaining healthy vessels and controling the development of atherosclerotic plaques.
“Smooth muscle cells also migrate during the formation of atherosclerotic plaque, and believe it or not, this is actually good,” says Lo Sardo. “Through migration these cells can make almost a blanket above the plaque and keep it from rupturing and causing damage. We think that by reducing their migration capacity, smooth muscle cells with the risk 9p21.3 could result in more unstable, deleterious plaques. So, taken together, you have cells that are not able to do vascular remodeling, not able to maintain a healthy vasculature, are prone to calcify and not promoting stable atherosclerotic plaques. I guess this is overall not an ideal mix.”
The human genome carries thousands of variants that increase the risk of developing CAD, but they are extremely difficult to study. Most of the time, like the 9p21.3, the regions are “gene deserts,” meaning they do not contain genes actively coding for proteins that make things happen in cells. The stem-cell approach used in the new study could help expose the effects of more of these disease-associated variants.
Clint Miller, a professor of genome sciences at the University of Virginia, helped confirm that the vascular cells made from induced pluripotent stem cells are a good overall match for smooth muscle cells in human arteries.
“They are remarkably similar,’’ says Lo Sardo. “This was an incredible result, because it makes us confident that whatever we find, it’s actually relevant, that we can faithfully recapitulate the biology of smooth muscle cells and their remarkable capacity to adapt to different stimuli just in a dish.”
This research was supported by grants from the National Institutes of Health (including T32GM007133), Chan Zuckerberg initiative, Silicon Valley Foundation, American Heart Association and UW–Madison.
Tags: genetics, stem cells




