Raw milk containing H5N1 can infect mice, while lab-based heat treatments greatly reduce the virus
Consuming raw cow’s milk that contains H5N1 avian influenza virus poses an infection risk, but a laboratory process that simulates high-temperature pasteurization reduces the virus in infected milk by more than 99.99%. That’s according to a team led by University of Wisconsin–Madison scientists, who reported their findings May 24 in a letter published in the New England Journal of Medicine.
The group, which also included researchers from Texas A&M University, found that mice that consumed untreated milk infected with H5N1 subsequently became ill with influenza and that small amounts of virus persist in untreated milk for weeks when kept at standard refrigeration temperatures. The research took place as the H5N1 avian influenza virus continued its spread from birds into mammals, with infections reported in dairy herds across the United States this spring.
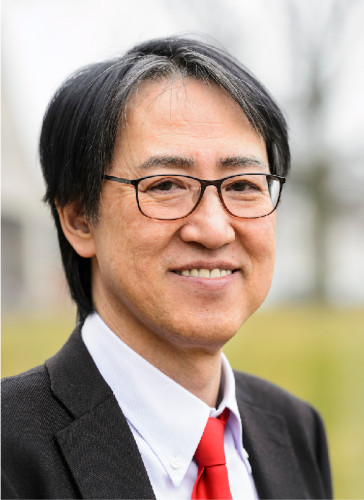
Yoshihiro Kawaoka, a professor in the UW–Madison Department of Pathobiological Sciences, and Keith Poulsen, director of the Wisconsin Veterinary Diagnostic Laboratory, led the work. The researchers tested two methods of heat inactivation on four H5N1-positive milk samples taken from infected cows in New Mexico and Kansas. Both methods were intended to simulate common pasteurization techniques, though the equipment and exact processes the researchers used differed from standard industry practices.
In the first, they heated infected raw milk to 145.4 F for a minimum of five minutes and up to 30 minutes. This method reduced the virus levels more than 99.999%.
The second method involved heating raw milk to 161.6 F for up to 30 seconds. This method inactivated more than 99.99% of the virus within the samples, though it did not completely inactivate the virus.
“We must emphasize that the conditions used in our laboratory study are not identical to the large-scale industrial treatment of raw milk,” says Kawaoka. “It’s important to remember that our heat-treatment findings may not perfectly translate to real-world conditions.”
Meanwhile, the team orally inoculated mice with untreated milk samples to gauge the possible risk posed by consuming raw milk that contains H5N1 virus. The mice began showing symptoms of illness after one day.
While no mice died as a result of infection within the experiment’s four-day window, subsequent analyses showed high levels of virus in their respiratory tracts, suggesting their infections originated in their throats. Some mice also had a significant amount of virus in their mammary glands, aligning with the high levels of virus found in infected cows’ milk.
To date, only two people in the U.S. have had confirmed H5N1 infections, one in Texas and another, reported May 22, in Michigan. Both cases were in farm workers who worked closely with dairy cattle, and the primary symptom in both was inflammation of the eye. While epidemiologists haven’t confirmed the mode of transmission, the Centers for Disease Control and Prevention said the most likely routes were from infected milk splashing into the workers’ eyes or from the workers touching their eyes with hands contaminated with the virus.
The latest findings suggest that people could also risk possible H5N1 infection if they consume raw milk from an infected cow.
“Do not drink raw milk,” says Kawaoka.