Mineral coatings could enable shelf-stable mRNA therapies
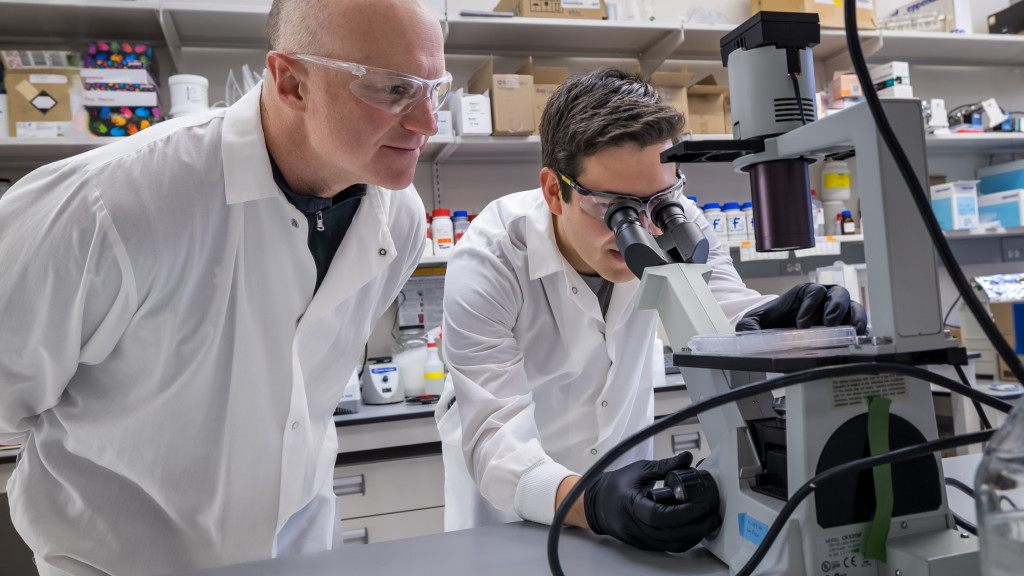
Professor William Murphy (pictured left) and collaborators in his lab, including Joshua Choe (right), have engineered a mineral coating that can maintain mRNA activity for up to six months at room temperature, with implications for wider and cheaper distribution of mRNA therapies, such as COVID-19 vaccinations. Photo: University of Wisconsin–Madison
A protective mineral coating identified by University of Wisconsin–Madison biomedical engineering researchers could allow powerful messenger RNA therapeutics like COVID-19 vaccines to be stored at room temperature, making them more accessible to lower-resourced communities across the world.
In a new paper in the journal Acta Biomaterialia, Professor William Murphy and collaborators in his lab detail how using an optimized mineral coating composition can maintain mRNA activity for up to six months at room temperature. With that kind of preservation, mRNA therapeutics — vaccines against infectious diseases, but also emerging treatments for cancer and tissue regeneration — could be stored on the shelf at local clinics.
The rapid development of mRNA-based COVID-19 vaccines was a gamechanger in the pandemic. The vaccines employ mRNA to direct cells to produce a protein from the surface of the virus, triggering an immune response that preps our bodies for the real thing.
Multiple estimates show the vaccines, a result of decades of incremental mRNA research — some of which resulted in a 2023 Nobel Prize — saved millions of lives.
There’s just one problem: The COVID-19 vaccines, as well as other mRNA-based therapies for cancer, require cold chain storage to maintain their potency.
“It sounds like a trivial problem, but it’s actually quite a tremendous problem,” says Murphy, a professor of biomedical engineering and orthopedics and rehabilitation. “If you’re trying to get these to sub-Saharan Africa, you’re going to have substantial challenges.”
Study lead Joshua Choe, an MD-PhD student in Murphy’s lab, screened 40 mineral compositions aiming to find one that, when combined with mRNA complexes, optimizes their stability in simpler formulations than those used for current vaccines. In the end, he identified a composition with a suitable amount of citrate and fluoride that maintained the potency of freeze-dried mRNA. He’s now applying the approach to similar formulations as those used in COVID vaccines with promising early results. The group has submitted a provisional patent based on the work through the Wisconsin Alumni Research Foundation.
“All the way to six months, you’re maintaining that activity, whereas without using our mineral to store those mRNA therapeutics, you lose quite a bit of the activity after two weeks, and then it declines to almost nothing,” says Choe, who hopes to work as an orthopedic surgeon and researcher after graduating.
The approach draws inspiration from ancient fossils’ documented ability to preserve DNA and proteins. Scientists successfully extracted DNA to analyze the genome of “Denny,” an estimated 90,000-year-old ancestor of humans whose remains were found in a Russian cave in 2012. In another find in Tanzania, researchers found intact proteins in ostrich eggshells that date to 3.8 million years ago.
Murphy’s lab has been using minerals to stabilize biological molecules for various biomedical applications for about 15 years, and Choe saw an opportunity to apply the tactic to mRNA therapeutics while working in the lab during the isolated days of winter 2020.
In addition to further demonstrating their approach’s effectiveness with mRNA vaccines, Murphy and his group are pursuing its use for tissue regeneration, particularly for treating spinal cord injuries, wound healing and regrowing cartilage, muscle and bone.
“We want to be able to achieve it in a way that comes off the shelf, so you can literally take a treatment off the shelf, apply it to a patient and stimulate tissue regeneration,” Murphy says.
William Murphy is the Harvey D. Spangler Professor and H.I. Romnes Faculty Fellow. He is also the founding director of the Forward BIO Institute at UW–Madison. Other authors on the paper include Murphy lab members Hannah Brinkman, a DVM/PhD student, and Jae Sung Lee, a staff scientist.
Funding for the research came from UW–Madison alumni philanthropists Mike and Mary-Sue Shannon as well as from the National Institute on Aging of the National Institutes of Health (award number F30AG077748 507), NIH award TL1TR002375 and the UW–Madison Medical Scientist Training Program award T32GM140935.