Banking on patient samples to advance COVID-19 research
In the spring of 2020, when instruction moved online and most research became remote, efforts picked up at the UW Carbone Cancer Center Translational Science Biocore BioBank. Researchers across campus began pivoting their studies to address the SARS-CoV-2 virus, which causes COVID-19. To do their research, they needed samples from patients.
They could find those samples at the TSB BioBank.
UW School of Medicine and Public Health immunologist Miriam Shelef, who focuses on better understanding rheumatoid arthritis to inform clinical care and treatments, was one of those researchers.
“When coronavirus COVID-19 came to the United States, and particularly Madison, people were shutting down their research labs. We had inadequate testing. We didn’t know if people were making antibodies or if treating people with convalescent plasma could be useful,” Shelef recalls. “There were many questions and no answers.”
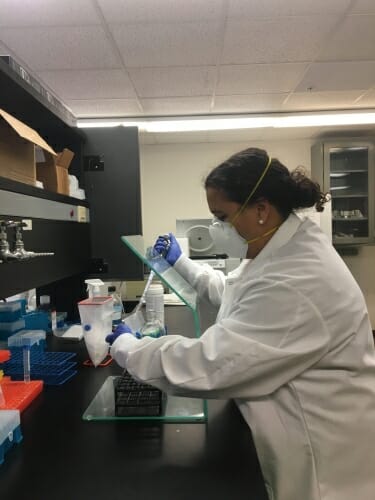
Aisha Mergaert, a graduate student in Miriam Shelef’s lab, is among several students who worked this summer to process samples for the COVID Convalescent BioBank. Courtesy of Miriam Shelef
To support COVID-19 research efforts on campus, she started sending emails in late March to see if anyone at UW–Madison was banking plasma or other blood products from patients recovering from the virus. Her group had previously established a biobank, or biological repository, of serum, plasma and other blood products from rheumatoid arthritis patients.
“No one knew of anyone doing that and so I got started,” says Shelef, a professor in the Department of Medicine.
Shelef applied for and received a research grant from the Wisconsin Partnership Program’s COVID-19 Response Grant Program, designed to help the university and community organizations across Wisconsin address the immediate health challenges of COVID-19. With the grant, she established the COVID-19 Convalescent Biobank, a biorepository for blood samples from individuals who have recovered from COVID-19. These samples include serum, plasma and immune cells.
Shelef worked with Betsy Nugent, chief clinical research officer for the School of Medicine and Public Health and UW Health, to initiate the project and received significant regulatory and coordination support from the SMPH Office of Clinical Trials. This includes individuals such as Mary Anne Kennedy, who heads regulatory efforts, and clinical research specialists Nolan Carroll and Jessica Van Bree, who helped with Institutional Review Board submission, recruitment, scheduling, consenting, sample collection, study visits and data collection.
“We are able to recruit subjects for this collection by identifying patients who have had coronavirus and then recruiting them five weeks after their symptoms have resolved,” explains Shelef. “At that point, they are no longer contagious and should have good antibody levels. We then collect longitudinally — five weeks, then three months and keep going out. With that, we can track if antibodies are long lasting, and the long-term immune response.”
In April, Shelef and Nugent reached out to Kristina Matkowskyj, an associate professor in the Department of Pathology and Laboratory Medicine, for help storing and distributing collections.
“My group was not equipped to decide who should get the samples and distribute samples, and they already had that infrastructure at the UW Carbone Cancer Center,” Shelef says.
Matkowskyj, who is now director of the UW Carbone Cancer Center TSB BioBank, also led the collection of samples from hospitalized patients acutely ill with COVID-19.
“In these cases, we have the initial nasopharyngeal swab samples used to make the diagnosis and the plasma and serum for these patients during their hospital course,” Matkowskyj explains. “We were able to reach out to our pathology colleagues and work with them to go ahead and pull samples that were going to be discarded from patients who were COVID-19 positive within the hospital and then transfer them to the biobank.”
Though the biobank is not currently recruiting new specimens, David Yang, professor of pathology and laboratory medicine, and Kornelia Galior, professor of pathology and laboratory medicine, assisted in running reports, pulling remnant nasal swab and blood samples from patients with suspected and confirmed COVID-19 infections, and transferring those specimens to the TSB BioBank. Collections could begin again as needed and acute sample collection is ongoing.
Gretchen Anding, assistant director of the Health Sciences Institutional Review Board Office, and her staff were instrumental in facilitating the changes to protocols and consents required for the TSB Biobank, including making connections to other COVID-19 registries and protocols. Patients, or their legally authorized representatives, must consent to their samples being used for research.
Matkowskyj also worked with Jon Audhya, SMPH associate dean for basic research, to create a centralized website where researchers could submit their research proposals for using COVID-19-related biospecimens. Audhya’s staff assembled a team for rapid review and approval to ensure distribution of samples according to scientific merit, technical feasibility and specimen inventory.
Initially, specimens were secured for UW research use, but the TSB Biobank was also able to share about 150 samples with the National Institutes of Health’s Vaccine Research Center.
The response from patients and their families has been positive.
“What I have heard from my amazing staff is that patient families — the patients who are in the ICU — want to help the next person, which we often find is the case with cancer patients who make donations,” says Matkowskyj. “In general, we have over a 95 percent consent rate for providing specimens to the biobank from those who have been approached and when it comes to COVID-19, I think it is even higher. I think people recognize the value and there is no additional cost to the patient or additional risk to the patient.”
The samples also offer valuable information because they are linked to clinical outcomes from the patients who provided them. Matkowskyj collaborated with Jomol Mathew, chief of biomedical informatics at SMPH and the Institute for Clinical and Translational Research, and Nasia Safdar, medical director of infection control at UW Health and professor of medicine at SMPH, to collect data, working with their existing registry of clinically curated respiratory illness cases. The dataset includes clinical information for COVID-19 positive and negative cases.
The biobank also provides investigators access to survey data and linked samples from other IRB-approved resources at UW, such as the Survey of the Health of Wisconsin, a statewide public health survey and biorepository. Working with Kristen Malecki, associate professor of population health sciences and co-director of SHOW, TSB BioBank is able to match COVID-19 patient samples with blood and DNA previously collected by SHOW, allowing researchers to identify environmental and genetic factors and biomarkers of risk, exposure and response to COVID-19 infection.
Students have also played an important role, says Shelef, including medical student Christopher Glover; graduate students Aisha Mergaert and Janna Bashar; and MD/PhD student, Maya Amjadi. They have volunteered to process samples, establish protocols, and extract clinical information from medical records. Amjadi has also begun COVID-19-related antibody research.
“This has truly been an institutional effort that mobilized quickly to enable this resource to become a reality for our researchers,” Matkowskyj says.
